An Abridged Photographic History of Organ Transplantation
Ignazio R. Marino, Claudia Cirillo
Abstract
Objectives: Organ transplantation is one of the most remarkable therapeutic advances in modern medicine; it started as an experiment and has become a life-saving practice. We briefly describe the major milestones of this multidisciplinary clinical science, the challenges that it still faces, and we consider the crucial contribution that its example could set for other medical fields.
Materials and Methods: A review of the literature was conducted and a selection of images was made to complete a brief history of organ transplantation, with a particular focus on liver transplantation.
Results: The largest problem affecting organ transplantation today is the shortage of organs. Attention should be given to preserving the peculiar high ethical value that characterizes the very nature of organ transplantation.
Conclusions: Methods successfully adopted by organ transplantation during the past 60 years can inspire promising fields, such as stem cell research, and provide useful tools to face the ethical challenges posed by scientific discoveries.
Introduction
Organ transplantation is among the most remarkable therapeutic advances in the past century. The therapy has progressed from clinical experiments to life-saving procedures. The development and success of organ transplant are associated with developments in other fields including surgery, immunology, critical care medicine, and infectious diseases. Bioethics and medical law have been affected by advances in organ transplant.
Ancient History
An interest in transplant is documented in mythology, religion, and art throughout human history. Descriptions of transplant procedures exist in Hindu texts dating from 2500 to 3000 BC, in which skin grafts cut from a patient’s own buttock or chin were used to reconstruct noses that were mutilated as a punishment for crimes committed.
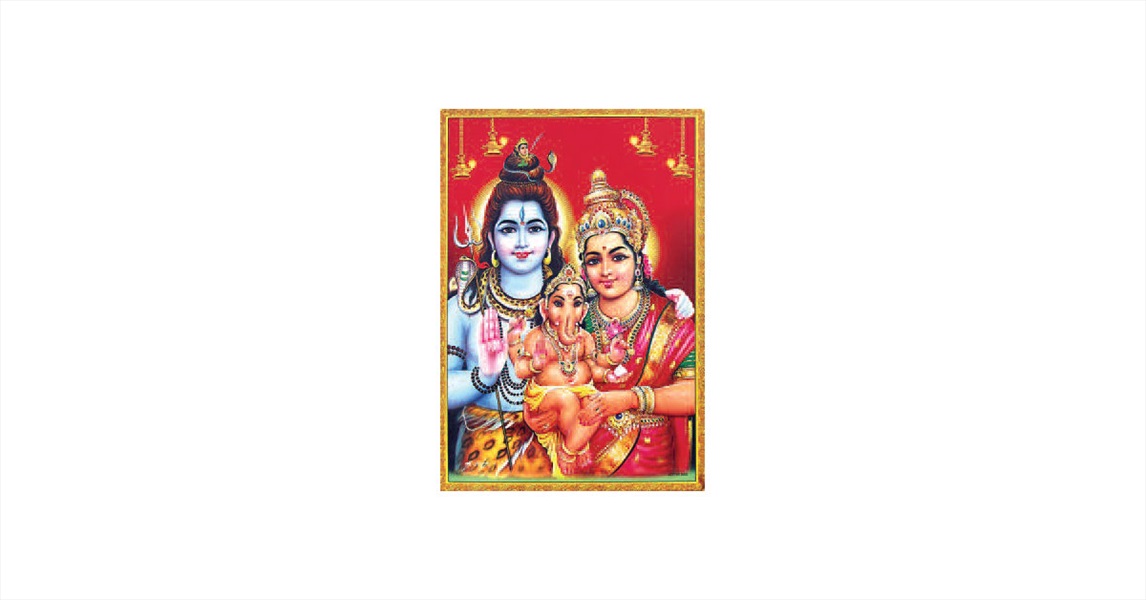
Lord Ganesha, in a myth from the 12th century BC, was the son of Parvati and Shiva (Figure 1). He was beheaded by his father while guarding the bath of his mother. An elephant’s head was attached to Ganesha’s body, bringing him back to life and making him the recipient of a successful transplant. The earliest known literary reference to a chimera was in Homer's Iliad. In Greek mythology, the chimera was a monstrous fire-breathing creature that had the head of a lion, body of a goat, and backside of a snake (Figure 2).
In a legend from China, the earliest Chinese physician, Pien Chiao, who died in 310 BC, exchanged hearts between a man of strong spirit and weak will and a man of weak spirit and strong will, to achieve a balance.
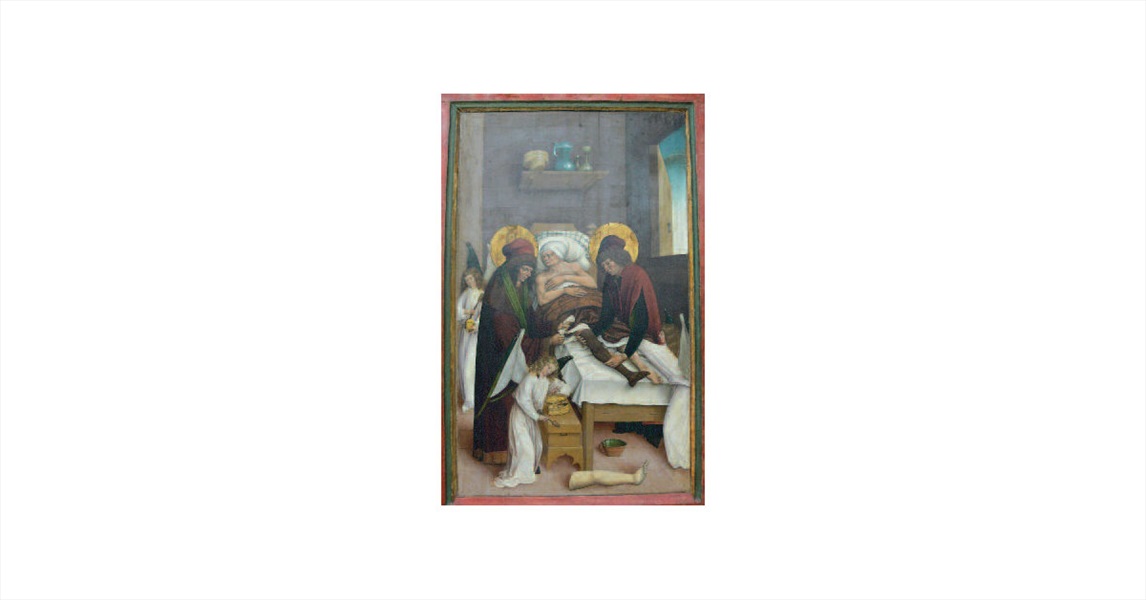
Several descriptions are found in the Bible that may be interpreted as a transplant. In Christianity, the “miracle of the black leg” was described in Jacopo da Varagine’s Legenda Aura (348 AD); in this transplant operation, the patron saints of surgeons, Cosmas and Damian, replaced a patient’s gangrenous leg with a leg from a recently deceased Ethiopian soldier (Figure 3).
Early Modern Transplantation
Clinical experiments in tissue and organ transplants gave hopes for transplanting as a therapy when Theodor Kocher (1841-1917), the Swiss surgeon, made the goiter operation a safe procedure. In July 1883, he transplanted thyroid tissue into a patient who had undergone radical thyroidectomy. This operation was an attempt to cure hypothyroidism by replacing an organ. It was the first known modern transplant and earned him the Nobel Prize in physiology in 1909 (Figure 4).
In Lyon, France, Alexis Carrel (1873-1844) transplanted a kidney from a dog’s abdomen to its neck (Figure 5). After moving from Europe to the United States, Carrel refined his surgical technique and developed the triangulation method of small vessel anastomosis. He was a Nobel laureate in 1912. Carrel also began collaborating with Charles Lindbergh (1902-1974) in 1930. Lindbergh was curious about developing a heart-lung machine to keep patients alive while surgeons operated inside the heart. Carrel and Lindbergh built the first known functional pump oxygenator that eventually led to the construction of the heart-lung machine (Figure 6).
After World War I and the Great Depression, research in organ transplantation continued. With the increased need for skin therapies for severe burns, the Brazilian-born English scientist Peter Medawar (1915-1987) investigated the mechanisms of skin allograft rejection (Figure 7). He discovered that skin grafts between monozygotic twins were tolerated. Rejection was understood as an immunologic phenomenon. Medawar was awarded the Nobel Prize in 1960.
The field of immunosuppression made marked progress with the collaboration of Gertrude Elion (1918-1999) and George Hitchings (1905-1998) that resulted in new chemotherapeutic drugs. Among these drugs, 6-mercaptopurine was improved by using sulphur-substituted compounds to create azathioprine. Azathioprine inhibited the immune response and was the only drug available for many years to prevent rejection.
Modern Clinical Transplantation
In 1954, the successful transplant of a kidney between living identical twins was performed by Joseph Murray (1919-2012) at the Peter Bent Brigham Hospital in Boston. The procedure was a surgical and immunologic success, and the recipient survived 8 years with no rejection. Murray was awarded the Nobel Prize in 1990 (Figure 8).
In the early 1960s, Thomas Starzl (born in 1926) at the University of Colorado showed that high doses of prednisone added to azathioprine could reverse kidney allograft rejection. This work transformed kidney transplantation into a successful routine procedure and led to the development of many centers of excellence in the United States and Europe. It also enabled the development of other organ transplants. Starzl inaugurated a liver program in Denver and performed the first successful liver transplant in 1967. In 1968, Sir Roy Calne (born in 1930) opened the world’s second liver transplantation program in Cambridge, England. Starzl and Calne established liver transplantation as a common therapy, perfected surgical techniques, and made major discoveries on immunosuppression. They shared the 2012 Lasker-DeBakey Clinical Medical Research Award for changing the field of organ transplantation and restoring normal life to thousands of patients with end-stage liver disease (Figure 9).
Other organ transplant advances during the 1960s included Keith Reemtsma’s (1926-2000) xenotransplant of a kidney from a chimpanzee to a woman who survived for 9 months. In 1963, a lung transplant was performed by James Hardy (1918- 2003) in a prison inmate who had a chronic lung infection; the patient survived only 18 days. Hardy also performed the first known animal-to-human heart transplant. A pancreas transplant was performed in 1968 at the University of Minnesota by C. Walton Lillehei (1918-1999).
The first known heart transplant was performed by Dr. Christiaan Barnard (1922-2001) in Capetown, South Africa (Figure 10); the patient, Louis Washkansky, was a 53-year-old Lithuanian immigrant who was diagnosed with myocardial infarction. Dr. Barnard had worked for 2 years at the University of Minnesota, where Lillehei was developing the field of open-heart surgery. Washkansky survived 18 days with his new heart; as a result, the operation was declared a success, and heart transplantation worldwide followed. There were 21 heart transplants performed during the first 6 months of 1968 in South Africa, the United States, England, India, France, Brazil, Argentina, Canada, and Chile, but results were poor.
The developments in organ transplantation procedures during the 1960s occurred, in part, because of a change in the definition of death. The previous cardiorespiratory definition of death had become inappropriate because of increased capabilities of intensive care life support technology. The concept of brain death was introduced in 1968 by a committee from Harvard Medical School. The report of this committee became influential, but debate about the contents of the report still persists.
Another major advance for transplant procedures was the discovery of the immunomodulatory properties of cyclosporine by Belgian immunologist Jean Borel (born in 1933) in 1977. Cyclosporine was introduced into clinical practice in 1978 and was approved by the United States Food and Drug Administration in 1983. In the early 1990s, FK506 (tacrolimus) was clinically investigated at the University of Pittsburgh by Starzl’s team in human liver transplant recipients who had rejection that was refractory to cyclosporine. The introduction of calcineurin inhibitors such as FK506 caused an improvement in graft and patient survival after liver transplant.
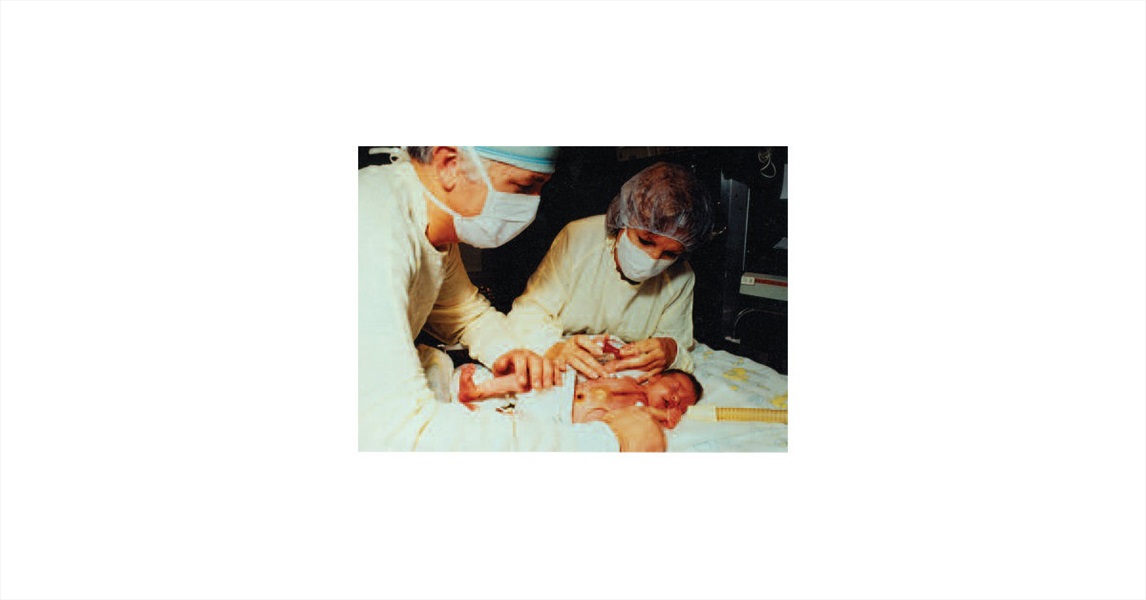
In October 1984, a 2-week-old baby girl (Baby Fae), who had been born with hypoplastic left heart syndrome, underwent a heart transplant with a baboon heart carried out by Leonard Bailey (born in 1942) at Loma Linda University Medical Center. This procedure was reported extensively in the lay media and was rather controversial (Figure 11). Starzl had performed the first known chimpanzee- to-human liver transplant in 1966. In 1992, his team at the University of Pittsburgh achieved patient survival for 70 days after a baboon liver transplant on a man. However, this experimental clinical trial was discontinued because of poor results. Although xenotransplantation may be a potential solution to organ shortage, it has been controversial since it was first attempted. Researchers continue to study new protocols for immune modulation and postoperative care, and the purpose of this research is to achieve long-term survival with solid organ xenografts.
Ethical Issues
Many advances in transplant procedures raise ethical questions. Ethical issues include organ supply and new diagnostic and therapeutic options. After decades of experimentation, organ transplants have been successful, and the primary issue at present is organ availability. Financial incentives for living- and deceased-donor organ donation have been suggested as a possible solution, but concerns exist about black market trade and abuse. To date, organ sale is illegal everywhere, except in Iran.
Conclusions
Transplantation is a field that has had many discoveries that have improved the lives of patients who have organ failure and other diseases. Many immunosuppressive drugs that were developed for use in transplants are also used to treat > 80 autoimmune diseases and several common allergic conditions. Methods that have been adopted in organ transplant procedures may inspire other fields such as stem cell research and may provide useful experience to address difficult ethical challenges posed by new scientific discoveries. Stem cell therapy has technical similarities with transplant procedures. The development of organ transplant procedures enabled treatment that surgery and pharmacology alone could not have achieved; stem cell research has similar potential. In the 1960s, organ transplant contributed to a new definition of death; current embryonic stem cell research may promote a global debate about the definition of the beginning of life. The unique symbolic value of transplant surgery is that its success requires solidarity, collaboration, and sacrifice. Altruism is an integral part of organ donation, hence of organ transplantation, and it remains a key principle for it. In no other surgical field does solidarity play such a crucial role. In no other clinical area are sacrifice and grieving turned into therapy and life so dramatically. Altruism, solidarity, and collaboration among different actors are particularly embedded also in the socioorganizational structure of transplantation, making the multidisciplinary aspect of it a replicable example for complex, emerging fields that raise profound ethical issues.
 06.60301809
06.60301809